Beyond Flipping a Switch: Generative AI at the Healthcare Application Layer
Examining Annual Wellness Visits as an AI Care Orchestration Use Case
Building on insights from a recent real-world clinical AI deployment conducted by OpenAI and Penda Health, this second article in our series takes a broader look at how the “application layer” – the interface between AI and clinical workflow – determines success. I wanted to focus on what I think is a perfect use case for agentic workflow in clinical care: Medicare’s Annual Wellness Visit (AWV). In this post I map out how integrating AI into this preventative care workflow can relieve operational burdens and unlock financial and clinical benefits.
Healthcare’s excitement about large language models has been palpable, but the key bottleneck now isn’t model capability – it’s implementation. In my last article, I examined the results of an early clinical deployment (the OpenAI–Penda Health study) that demonstrated AI’s potential when carefully integrated. Now, we zoom out to look at how generative AI can be embedded into daily care delivery. Nowhere is this more apparent than at the application layer – the user-facing workflows and tools that turn a clever model into tangible improvements in outcomes and efficiency.
Annual Wellness Visits: A Perfect Use Case for Generative AI
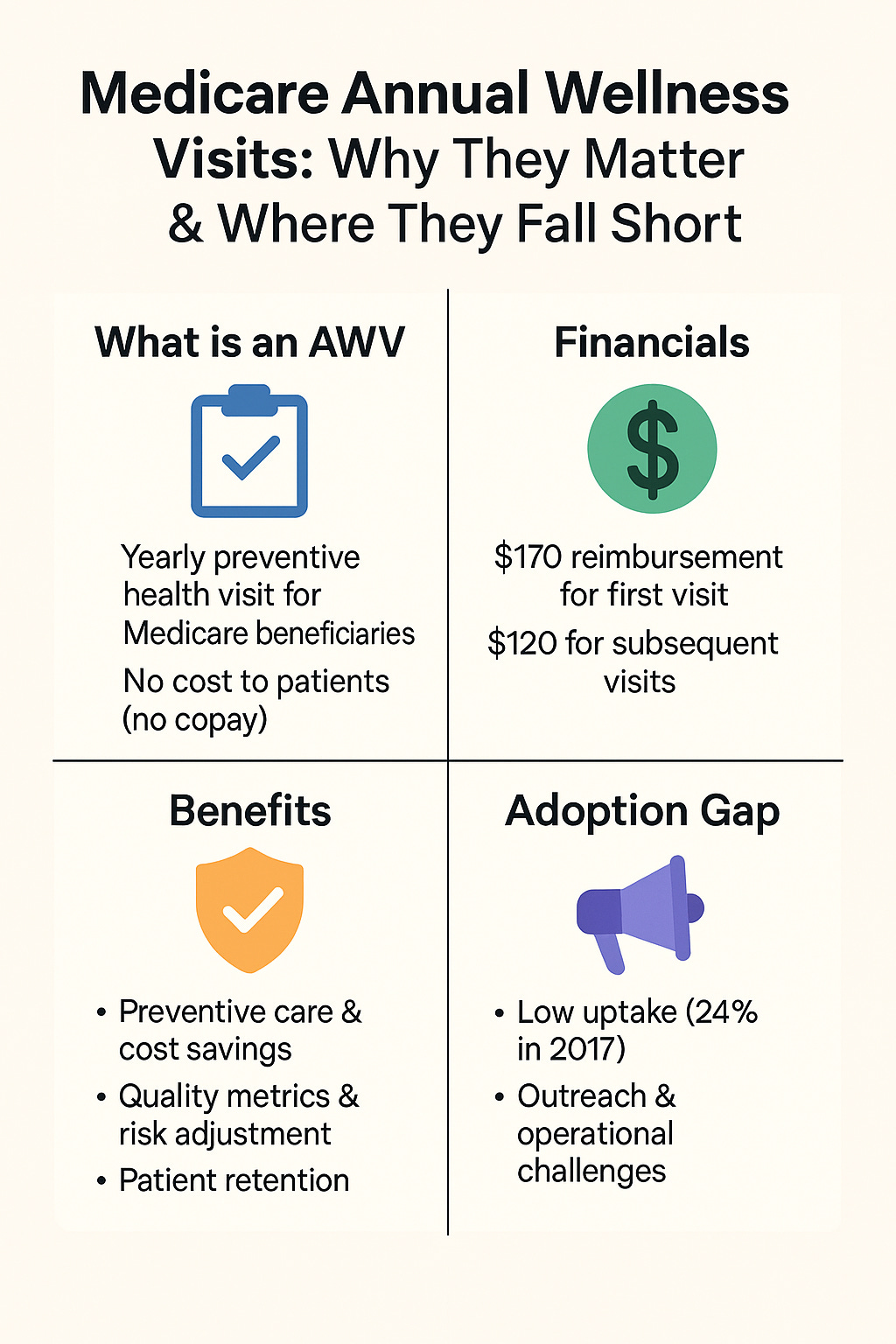
The Medicare Annual Wellness Visit (AWV) is an ideal scenario to illustrate the power of generative AI in healthcare. Introduced in 2011, the AWV is a yearly preventive health visit for Medicare beneficiaries, intended to focus on health maintenance, screenings, and personalized prevention planning. AWVs come at no cost to patients (no co-pay) and are reimbursed by Medicare at a relatively high rate (approximately 2.43 RVUs for the first AWV and 1.5 RVUs for subsequent annual visits, roughly $170 and $120 respectively). Beyond the direct reimbursement, AWVs offer several financial and clinical advantages for providers and health systems:
Preventive Care & Cost Savings: AWVs ensure patients receive evidence-based screenings and vaccinations that might otherwise be overlooked. Studies have linked AWVs to increased uptake of preventive services (like cancer screenings and immunizations) and even modest reductions in downstream costs – one analysis found first-time AWV patients had a 5.7% reduction in total healthcare costs over the next year. (Though evidence is mixed, the intent is to catch issues early and reduce expensive complications.)
Quality Metrics & Risk Adjustment: The structured AWV format helps close care gaps and document chronic conditions. Data collected can satisfy quality measures for value-based care programs. Accurate documentation of diagnoses (e.g. capturing HCC codes for chronic conditions) during AWVs can raise patients’ risk scores, translating to higher reimbursements for sicker patients in Medicare Advantage or ACO programs. In essence, AWVs help providers “do well by doing good” – improve care while also maximizing performance metrics and revenue.
Patient Retention and Attribution: An AWV is an additional touchpoint binding the patient to the practice. Completing an AWV can solidify a Medicare patient’s attribution to a provider in an Accountable Care Organization, which is important for continuity and shared savings calculations. It’s also an opportunity to build patient rapport in a non-acute context. This is a critical point.
Despite these benefits, AWV adoption has been far lower than expected. Only about 24% of eligible Medicare beneficiaries received an AWV in 2017 (up from 7.5% in 2011), meaning roughly three-quarters of seniors miss out on this preventive service. That low uptake represents millions of missed opportunities for preventive care and significant unrealized revenue for practices. The reasons are largely operational. Conducting AWVs at scale is hard. Primary care clinics face numerous practical challenges in trying to expand AWV volume:
Patient Outreach & Scheduling: Identifying hundreds (or thousands) of eligible patients and getting them scheduled is labor-intensive. Clinics often resort to call campaigns, mailed letters, and manual follow-ups. Even well-resourced systems have needed to create worklists, hire care coordinators, and offer incentives just to boost AWV rates modestly. Every step – from convincing patients to come in, to finding an appointment slot – is a hurdle.
Pre-visit Data Gathering: Patients are supposed to fill out a Health Risk Assessment and provide updates on their history as part of the AWV. Without assistance, either the patient arrives with incomplete information or staff must spend time collecting data via forms or calls beforehand. This can easily consume staff hours.
Lengthy Visit & Documentation: An AWV covers a lot of ground – medical/family history, medication review, vitals, cognitive and depression screening, functional assessment, preventive counseling, and more. Ensuring all 20+ required elements are addressed and documented in the EHR is a heavy lift for clinicians, who already feel pressed for time. One vendor estimates that end-to-end, an AWV can demand 45+ minutes of staff time just in paperwork, data entry, and coordination.
Follow-up Coordination: The “output” of a successful AWV is a Personalized Prevention Plan – essentially a to-do list of referrals, screenings, or lifestyle interventions the patient should do. Chasing down these next steps (scheduling mammograms, referring to specialists, enrolling the patient in programs) creates another layer of work for care teams.
Even for organizations that invest in customer relationship management (CRM) systems and employ care navigators, scaling this process to an entire Medicare panel is daunting. Many practices simply lack the bandwidth to systematically engage every eligible patient, so AWVs end up done opportunistically or not at all. This is where generative AI can shine. The repetitive, communication-heavy, checklist-driven nature of Annual Wellness Visits makes them a perfect use case for LLMs and AI assistants.
Generative AI, embedded in a well-designed application, could tackle the major pain points above by functioning as a virtual clinical assistant for AWVs. Instead of relying solely on human staff to conduct outreach, data collection, documentation and follow-up, an AI-powered system can automate and enhance much of this workflow. For example, an AI could proactively reach out to every eligible patient with a personalized invitation (via text, email, or patient portal) explaining the benefits of an AWV in plain language. It could then converse with patients asynchronously to gather their health updates and answer common questions – much as a human medical assistant might, but available 24/7 and at scale. All of this information can be compiled and summarized before the patient ever sets foot in the clinic. The capacity of AI to engage patients outside of visits without increasing staff workload opens up new possibilities to finally execute population-wide outreach like AWV programs effectively.
Step-by-Step: AI-Enhanced Annual Wellness Visit Workflow
To make this more concrete, let’s walk through how an AI-assisted AWV program could work in practice. The following illustrates a step-by-step workflow blending generative AI into each phase of the Annual Wellness Visit process:
Identifying & Inviting Eligible Patients: The system automatically identifies Medicare patients due for their yearly AWV (for example, by scanning the EHR for those who haven’t had one in 12 months). It then sends a personalized outreach message via the patient’s preferred contact method (text, email, portal) inviting them to schedule their AWV. The message, drafted by an LLM in a friendly, easy-to-understand tone, emphasizes why the visit is important (e.g. “to review your medications and screenings and keep you healthy”) and addresses any misconceptions. (In organizations with value-based contracts, every patient who completes an AWV contributes to quality metrics and revenue – making robust outreach financially worthwhile.) If the patient is interested, the AI can even assist with scheduling – for instance, by presenting available appointment slots or initiating a call with the clinic. This eliminates phone tag and reduces barriers to booking the visit.