Designing a Patient Self-Reporting Stack Around Humans and AI
Patient engagement is a pillar of care transformation but the digital door is broken. Can AI fix it?
I’m excited this week to share a deeper dive on what we’re building at RevelAi Health. My Co-Founder and legendary Chief Technology Officer
wrote up an excellent blog post on the power and problems of patient reported outcome measures. His initial post is on his blog, and we’re excited to showcase it here on The Techy Surgeon as well.Every care team we talk to has some version of the same complaint: patients like to engage by text, they call and leave voicemails, they will fill out countless surveys, but those signals rarely make it into the plan of care.
Electronic records were never built to absorb this ambient context, and the people who could act on these streams of communication are already drowning in portal messages and follow-up calls. The value of changing this paradigm should be obvious. Timely symptom reporting keeps people out of the ED, surfaces social needs, and lets providers adjust therapeutic plans before a flare turns into a crisis.
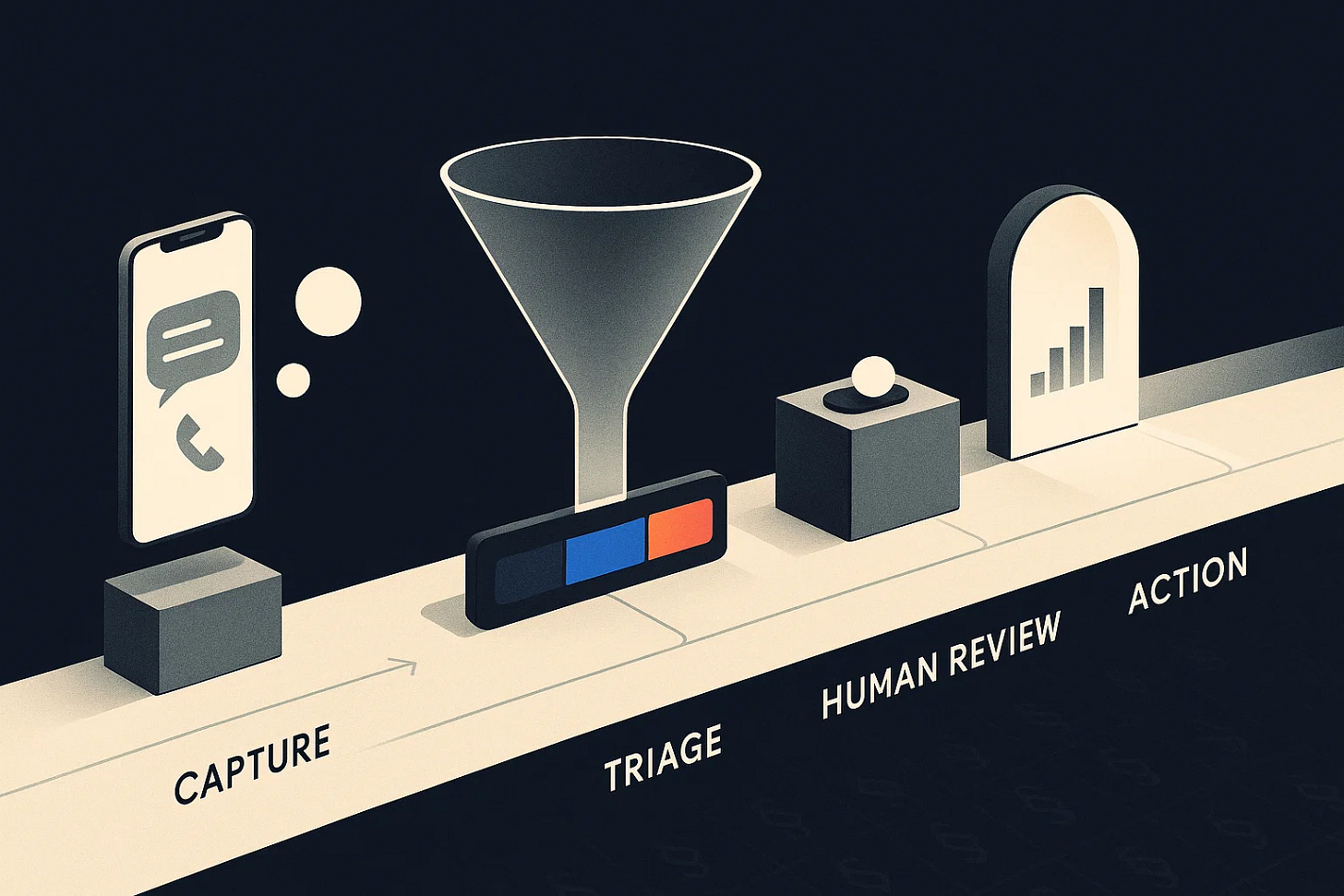
But what we need is a stack that captures self-reported data, triages it with large language models, and still gives clinicians the last word. The winning pattern blends thoughtful UX, observability, and a human-in-the-loop workflow.
From raw patient signals to a governed handoff: capture → LLM triage → human review → documented action.
Where Patient Self-Reporting Stands Today
Remote symptom logging works when someone is watching. In the RELIEF pilot, oncology patients completed 80% of daily check-ins and nurses intervened on half of the triggered alerts, zero symptom-related ED visits during the study window (Curr Oncol, 2021).
PROM and PGHD programs still stall in pilots. An umbrella review catalogued fractured adoption because implementation teams underinvested in workflow design, training, and staff capacity (Syst Rev Protocol, 2024).
Integrating patient-generated data into the EHR is barely out of the lab. Only 19 studies met the bar in a 2019–2021 scoping review for inclusion, most of them diabetes pilots that cited resource load and inconsistent review patterns as blockers (JAMIA, 2021).
Portals add work faster than they add value. Cleveland Clinic primary care teams saw quarterly message volume double (340 → 695) and every 10 extra messages meant ~12 minutes more after-hours EHR time (J Gen Intern Med, 2024). Duke University School of Medicine’s Orthopedic surgery department recently published a staggering study showing that EHR inbox volume has increased 13,000% in the same period surgical volume increased only 2x.
The signal could be rich, but the stack for sorting this brand of data is brittle. We ask patients to speak to us through multiple unstructured modalities, and then make it the nurse’s job to find needles the haystack.
Why the Workflow Breaks
Fragmented entry points: IVR trees, unsecured SMS threads, phone tag with call centers, and app-based chatbots all capture different slices of the story with no shared state.
Review is entirely manual: care coordinators listen to voicemails, gather context from the chart, and often re-document disparate data points into the system of record from multiple entry points.
Outbound outreach is slow: when everything needs a human touch from scratch, the bottleneck makes patients feel ignored and high-acuity cases are delayed.
No closed loop: patients don’t hear back quickly, so engagement drops, satisfaction plummets, unnecessary alarm and acute care utilization increases; meanwhile clinicians don’t trust the data, so they stop looking.
We can’t fix this by “adding AI” to a broken assembly line. We need to reframe the patient self-reporting stack as an orchestration problem.
Patterns for a Human-Centered Self-Reporting Stack
1. Intake that sets expectations up front
Large language models can score acuity quickly and accurately (VUMC’s retrieval-augmented triage hit 0.98 sensitivity JAMIA, 2024).
Patients are given a commitment (“a nurse will join in under a minute if needed” or “we’ll text you an answer in two hours”), which keeps engagement high.
2. Inbox triage that surfaces context, not noise
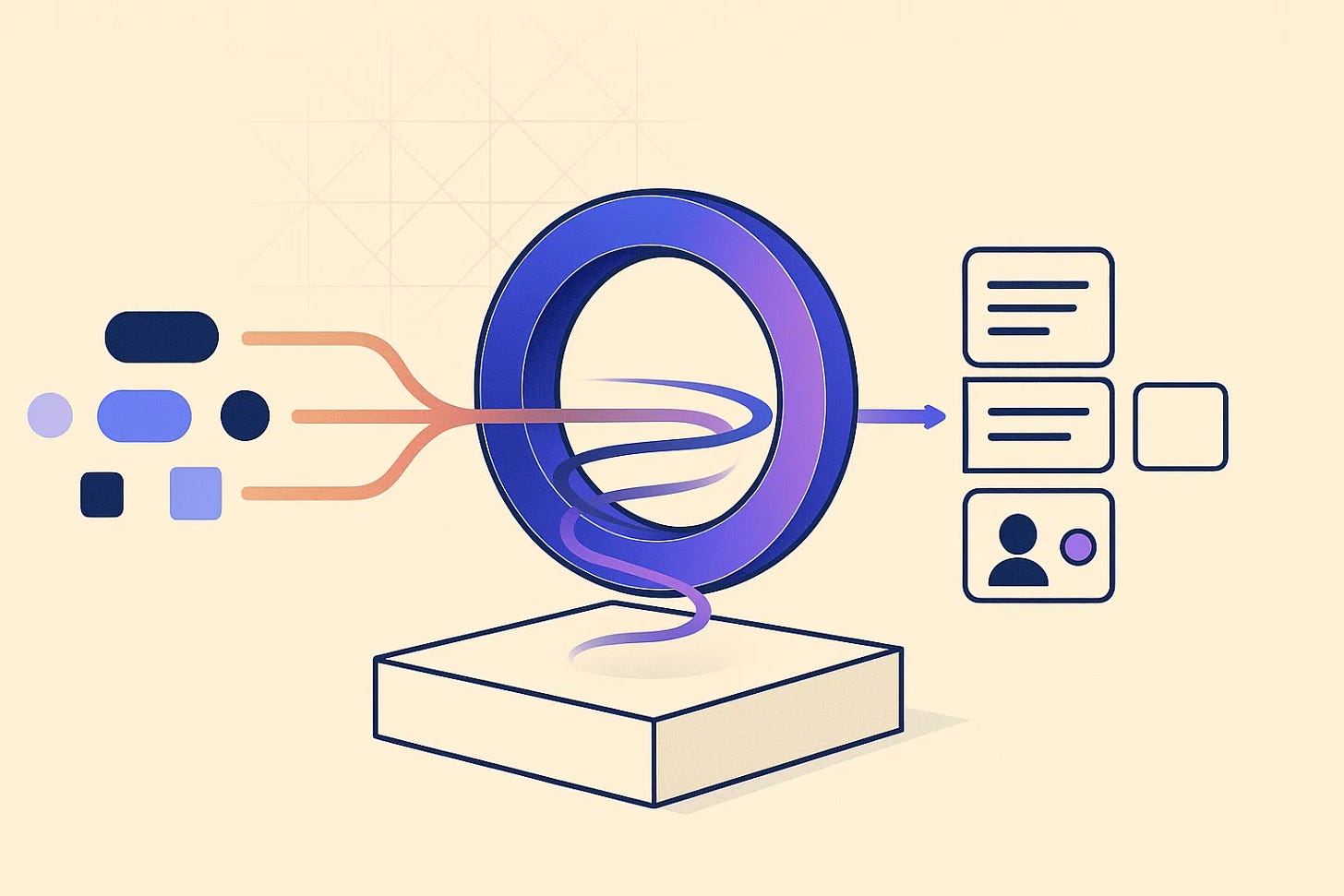
KIMI (Knowledge Informed Management Interface), is RevelAi Health’s Large Language Model based Clinical AI Co-Pilot and Triage Agent
Inbox views should group by intent (med refill, wound concern, paperwork) and stack related history—last summary, vitals, social determinants callouts.
Drafting LLM replies isn’t about replacing clinicians; Mayo Clinic teams used AI drafts in ~20% of portal responses and reported lower task load afterward (JAMA Netw Open, 2024).
Auto-resolution stays limited to low-acuity scripts (e.g., PT protocol reminders) and still leaves an audit trail.
3. Outbound nudges that feel bespoke
Aggregated self-reports feed longitudinal trends (pain scores, medication adherence, social needs). When a metric drifts, the orchestrator drafts follow-up language tailored to that patient’s literacy and history.
Humans confirm the plan, especially when it involves medication changes or complex counseling.
4. A shared workspace with observable loops
Every automated action should show provenance: which notes were summarized, how the LLM scored acuity, and who signed off.
Dashboards for clinical leaders track alert volume, average time to human response, and which prompts drive escalations.
Patients see status indicators (“reviewed by triage nurse at 3:12 PM”), reinforcing trust that their data matters.
How LLMs Help, When They’re Tethered to Humans
LLMs earn their keep by shrinking the research burden on the care team:
Context gathering: assemble medication history, recent labs, and prior outreach before a human opens the chart.
Summarization loops: recursive summaries keep cross-channel interactions digestible without losing dosage details or timelines.
Acuity classification: flag high-risk language inside texts and voicemails instantly, so humans act faster.
Drafting outbound communication: suggest responses that a nurse can approve or tweak in seconds.
But they always operate inside a governed loop. High-acuity cases trigger synchronous handoffs. Every draft carries a “source disclosure” showing the snippets the model used. Clinicians can thumbs-up or correct the draft, feeding evaluation back into the system.
Translating Agentic Workflows to Care Transformation
In value‑based contracts, the early post‑discharge window concentrates avoidable utilization. A conversation‑first engagement layer turns those patient signals into Transitional Care Management that actually happens: the agent confirms discharge in plain language, reconciles medications from chart context, books the 7–14‑day visit in the same thread, and routes any red‑flag phrases to a human within minutes. The same playbook helps pre‑op. If a joint‑replacement patient repeatedly skips readiness assessments or leaves a distressed voicemail, the system tags “early‑intervention,” prompts a navigator call that solves transportation or medication confusion, and swaps in a tele‑visit when needed. These are the touches that move outcomes; among Medicare beneficiaries, receipt of TCM is associated with lower short‑term costs and mortality.
PROMs and patient‑generated data work best when missingness is treated as a clinical signal. The agent makes completion feel human—“Would you rather text or talk? It takes two minutes”—then, after two missed pings, automatically buckets the patient for navigator outreach. From there, campaigns are concrete: close missed follow‑ups, establish primary care, schedule the Annual Wellness Visit, and line up preventive screenings; for ED diversion, concerning symptom language triggers same‑day coaching and an urgent clinic slot. Boards can read this on one page: completion rates, time‑to‑first human touch after a concerning signal, and gap‑closure by segment. Randomized trials show that systematic electronic symptom monitoring improves quality of life and reduces unplanned use when tied to real‑time follow‑up—the exact loop this design operationalizes. (Steinbeck et al.)
What We’re Building at RevelAI Health
At RevelAI Health, we are stitching these patterns together so health systems don’t have to bolt on yet another point solution. Our orchestration layer listens to phone triage, portal inboxes, and AI-assisted callers, runs LLM-based acuity and intent models, and hands the care team a structured summary with suggested actions. Humans always close the loop, but they start from a prepared canvas instead of a blank screen.
The payoff is simple: patients know someone is listening, care teams spend time on judgment calls instead of transcription, and leaders can finally measure whether self-reporting is reducing avoidable visits.
Incumbent EHR vendors Epic, Cerner, the rest of the club certainly have the data gravity to tackle this, and they own the workflows inside the chart. But their strength on in-visit and inpatient documentation has not translated into nimble inbound and outbound engagement. Telephony integrations remain bolt-ons, multi-channel intent routing is brittle, and most of the tooling still assumes a human will manually stitch the story together.
We’re still refining evaluation datasets, UI treatments, and human review workflows—but the stack is finally showing that AI and thoughtful UX can make patient self-reporting actionable without losing the heart of human-centered care.
If you’re experimenting with your own self-reporting stack, we would love to compare notes. The work ahead is making these loops tight, auditable, and empathetic.







As a patient and advocate for my family members, I would love to see this come to life across the U.S. healthcare system. Just went through several examples of sending text messages, messages in provider portals, and phone calls only to have to repeat it to the provider in person. Feels like you're on the right track for sure.
While we're not experimenting with a self-reporting stack like yours, we are experimenting with a way to turn in-depth articles like yours into quick, shareable videos. The kind that will help posts like yours reach a broad audience and drive them back to your post.
We shared one earlier today that we hope is a fair reflection of your post.
https://biteable.substack.com/p/substack-daily-finds-2025-10-03
I think healthcare should just read their emails. Lol