You’re Using Your Clinic’s Ambient Scribe Wrong
A guide to maximizing the impact of ambient technology on clinical documentation
Ambient AI scribes – the technology that automatically transcribes and summarizes doctor-patient conversations – have swept through healthcare in the past two years. Nearly one-third of physician practices now use some form of ambient scribe, often integrated directly into their EHR systems[1][2]. For any clinician drowning in the usual laborious heap of administrative burden, the appeal is obvious: these tools dramatically reduce documentation workload, giving doctors more time with patients and less time tethered to keyboards. Studies show ambient AI scribes can cut documentation time by 20–30% and after-hours charting (“pajama time”) by about 30%[3]. In a recent multicenter trial, physicians using an AI scribe for just one month saw their burnout rates drop from 51.9% to 38.8%, a significant improvement in well-being[4]. Even patients notice the difference: in one rollout, 47% of patients said their doctor spent less time staring at the computer, and over half felt the quality of their visit improved with an AI scribe on board[5].
This promise of efficiency and renewed focus on patients has driven unprecedented adoption of this technology. One large health system deployed ambient scribes to 7,000+ physicians who documented 2.5 million encounters in just over a year[6]. Venture capital is also pouring fuel on the proverbial fire. In 2025 alone, multiple AI scribe startups landed blockbuster investments soaring to billion dollar valuations. Abridge, arguably the leading ambient documentation company, raised $300 million in a Series E round (just months after a $250 million Series D), boosting its valuation to $5.3 billion[7]. Ambience Healthcare secured $243 million in Series C funding co-led by Oak HC/FT and Andreessen Horowitz[8], and Heidi Health just closed a $65 million Series B (valuing the Australian-based scribe platform at $465 million)[9]. With tech giants and startups alike in the fray (Microsoft’s Nuance DAX, DeepScribe, Suki, and others), ambient scribing has quickly become big business.
Yet for all the hype, I’ve observed that many clinicians are not taking full advantage of what ambient scribes can do. As an early adopter, I participated in an ambient scribe pilot and commercial roll out of Abridge at Duke in late 2024 and have used one for nearly 100% of my clinic notes since. I’ve seen colleagues fall into two camps. Some aren’t aware of the technology’s capabilities and therefore hardly use it. Others switch it on, but stick to their old documentation habits, under-utilizing the AI or using it in clunky ways. The reality is that we’re often using our clinic’s ambient scribe wrong. We’re treating it like a passive dictation device, when it can be so much more.
Consider this common approach to ambient scribe adoption: a physician walks into the exam room and says a brief introduction to the patient along the lines of, “Just so you know, I’m using a recording assistant that will help write our note.” They then conduct the visit, maybe speaking a bit more verbosely than normal – explicitly stating lab results, assessments, and the care plan for the microphone’s sake. The ambient scribe duly produces a draft note capturing what was said. This does work; you’ll get a serviceable note in many cases. But it can feel awkward and unnatural. No patient enjoys hearing their doctor drone, “Your hip internal rotation is 30 degrees, sensation intact to light touch in the S1 distribution,” as if reading off a checklist. Over-narrating every exam finding or typing mnemonic makes the conversation stiff. The magic of ambient scribing, that it can fade into the background, is lost if we turn our patient encounters into dictated monologues.
In my experience, there’s a better way. Below, I’ll share some tips and techniques to truly harness ambient scribe technology. Think of it as moving from using a basic “Dictaphone” mindset to a more interactive, AI-enhanced workflow. With a few adjustments, you can make your ambient scribe produce better notes with less effort, all while keeping your patient interactions natural and human. (And don’t worry – you don’t have to abandon your beloved dot phrases or templates in the process.) Before diving into the how-to, one quick note on privacy: yes, these systems are HIPAA-compliant, and patients should be informed that the visit is being recorded for documentation. In many U.S. states, one-party consent laws mean it’s legally sufficient for the clinician to consent to the recording, but ethical practice dictates getting the patient’s permission as well[10]. Most patients are fine with it – especially when you explain it helps the doctor focus on them instead of the computer – but they appreciate the transparency about how the audio is used and stored[11]. With that settled, let’s get into making the most of your ambient AI scribe.
Tip 1: Customize the AI’s Note Style (Don’t Settle for Default)
One of the most powerful (and under-used) features of ambient scribes is the ability to customize the output. Many ambient documentation tools allow you to create custom templates or adjust the style and format of the notes they generate. In practice, this means you can prompt the AI on how you like your notes written. For example, you might prefer a concise narrative paragraph over a list of bullet points, or vice versa. Perhaps you want the Assessment & Plan section to start with a one-line summary followed by numbered plans, or you like your Review of Systems in a particular order. Don’t assume the AI is a black box. In many cases you can configure your note preferences.
How do you do this? Typically, in the ambient scribe’s settings or dashboard, there’s an option to create a custom note template. This isn’t a template in the old “copy-paste” sense, but rather a set of instructions (a prompt) and examples for the AI. You might write something like: “Format the note in full sentences, use a formal tone, and group the assessment and plan by problem.” Some systems even let you save multiple styles (for instance, Detailed vs. Concise) and toggle between them. In my experience, the ambient scribe from Abridge has struck a nice balance here, offering both a detailed narrative or a lean summary format at the user’s choice. The key is that you’re in control of the note’s voice and verbosity. At default settings, some AI-generated notes can be overly verbose – drowning in irrelevant detail – while others swing too far toward skeletal bullet points. By setting up your own template, you can hit the sweet spot that suits your specialty and personal documentation style.
This customization isn’t just for aesthetics; it has real workflow benefits. If the AI’s first draft is closer to how you ultimately want the note, you’ll spend less time editing. For example, if you hate when the note says “Patient denies X, Y, Z” in a single paragraph, you can prompt it to itemize negatives in a list or to omit trivial negatives altogether. Over time, a well-tuned AI template can save you significant clicks and keystrokes. Think of the ambient scribe as a junior colleague who can be trained: it will draft notes in whatever style you teach it. So don’t hesitate to dig into the settings and train your scribe.
Evidence check: If you’re worried that all this is more trouble than it’s worth, consider data from early adopters. At Kaiser Permanente, where thousands of physicians use AI scribes, one barrier for some holdouts was “lack of integration with note templates” – essentially the fear that the AI’s output wouldn’t fit their documentation style[12]. The physicians who got past that and customized the tool reported that it “significantly reduces the time to complete documentation,” making their lives easier both at work and at home[13]. In other words, a little upfront customization can pay off in spades.
Tip 2: Use a Hybrid Note – Combine AI Drafting with Your Templates
Let’s dispel a common misconception: adopting an ambient scribe does not require throwing out all your tried-and-true documentation templates. In fact, one of the smartest ways to use an AI scribe is a hybrid approach – let the AI handle the free-text heavy lifting for certain sections of the note, while you retain your own structured text or “smart phrases” for the rest. If you love your bullet-form ROS or the specific wording of your exam template, you can keep using them. Simply insert the AI-generated portion where you want it.
Most ambient scribe platforms and modern EHRs support this kind of integration. For example, if you use Epic or Athenahealth, you can often create a special dot phrase (like .AISCRIBE) that, when inserted into your note, pulls in the AI scribe’s output for a given section. Perhaps you’ll configure your clinic note such that your usual template populates all the standard fields (history, meds, etc.), and you leave a placeholder for the AI to drop in the History of Present Illness (HPI) narrative or the Assessment/Plan. This way, you get a seamless blend: the note reads partly in your familiar voice and format, and partly as drafted by the AI from the conversation. I often reassure colleagues, “You can use the scribe just for the parts you want help with, and keep the rest of your note exactly the way you like it.” Many are surprised – you can 100% do that! – because they assumed the AI would overwrite everything.
From a workflow standpoint, this hybrid method can be the best of both worlds. It addresses a major adoption hurdle: physicians worry that editing a full AI note might take more time than simply typing their own[12]. But if the AI is only drafting, say, the Subjective and Plan, and you’re otherwise relying on your trusty template text for Objective and Assessment, you have far less to review and edit. Indeed, ambient AI pilots have found that integration into existing workflows is key. In the Kaiser study, some low-use physicians perceived editing the AI note as burdensome – but the fix suggested was better customization and integration into their normal templates[12]. In practice, once doctors learn they can slot the AI’s content into their notes with a simple command, many of those reservations disappear.
How technically you do this will depend on the system. Some ambient scribes produce a structured output already divided into sections (SOAP format), which makes selective use easy. If it’s an embedded solution (like Nuance DAX in Epic), it might auto-populate discrete fields in the EHR. Other times, you might copy-paste from a standalone app into your note. Even in the latter case, you can copy just the portions you need. The point is to marry the AI’s strengths with your preferences. You get to maintain certain phrases or billing-required language that you know needs to be there, while offloading the bulk of narrative writing to the machine. I’ve seen clinicians who said, “I’m married to my template,” become much more open to ambient scribing when they realize they don’t have to divorce their template – they can simply augment it.
One more benefit: using the hybrid approach can alleviate the concern that AI notes might omit required elements. For instance, if your compliance department insists on a specific disclaimer or phrase in every note, keep that in your template. Let the AI fill in the rest around it. Until AI scribes are savvy enough to automatically include all the nuanced compliance verbiage (we’re not quite there yet), this approach ensures nothing gets missed. And speaking of missed details…
Tip 3: Talk to Your AI Scribe – Before, During, and After the Visit
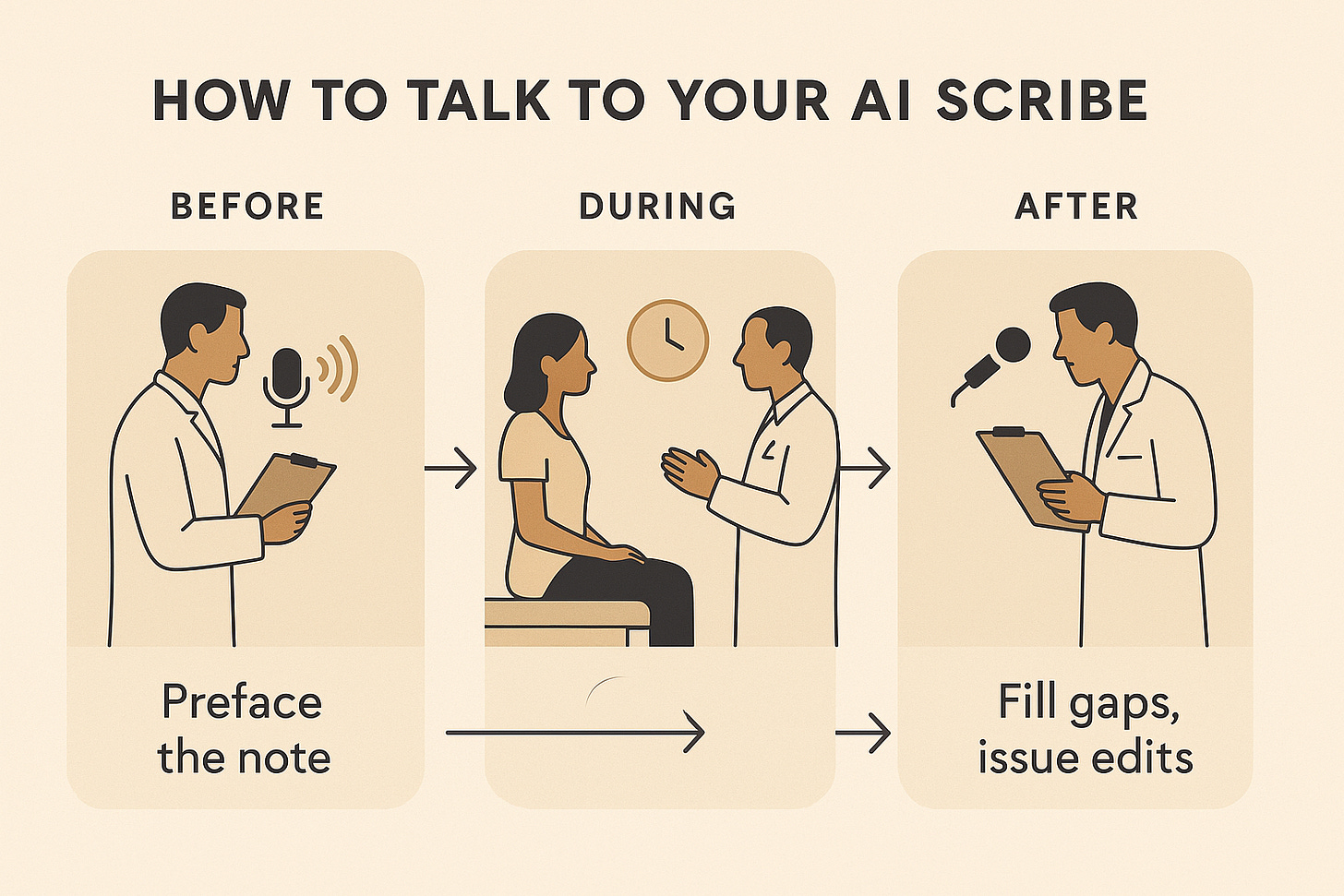
Perhaps the biggest leap in using an ambient scribe effectively is learning to communicate with it as you would with an assistant. This means embracing an “expressive voice” workflow – essentially narrating to the AI when appropriate – instead of either staying mute or, conversely, awkwardly dictating everything in front of the patient. Done right, this approach lets you capture a richly detailed note without compromising the patient’s experience. Here’s how I do it:
Before entering the room, pre-chart verbally: I start the ambient recorder and give a quick preface about the patient’s background for the AI’s ears. For example, while reviewing the chart, I’ll say into the microphone (in a low voice or even outside the room): “Preface for the note: this is a 38-year-old male with a history of diabetes, COPD, and hypertension. He was hospitalized last month (July 7, 2025) for pneumonia and had surgery on [date].” In essence, I feed the AI the context that I normally carry in my head, so that the note will be properly framed. Then I pause the recording. This step takes perhaps 30 seconds of speaking, but it can save me from later manually inputting the past medical history or hospital follow-up details. Remember, you can speak much faster than you can type – humans average about 150 words per minute speaking versus ~40 wpm typing[14] – so talking this info in is a quick win.
During the encounter, focus on the patient (with light narration): I resume recording when I enter the room and then pretty much forget about it. I have a normal conversation with the patient. I do not turn into a narrator of every physical exam finding. The key is to stay natural. I might still be a bit more detailed than I’d be without a scribe (e.g., saying “Let’s check your knee reflex which looks normal” instead of silently clicking my hammer), but I won’t bombard the patient with medical jargon. I trust myself to remember certain exam details that I can add later if needed. What I do make sure to verbalize clearly is the Assessment and Plan. Ambient scribing, I’ve found, forces you to be more explicit in explaining the plan to the patient, which is actually a great thing for communication. For instance, I’ll say, “So to recap, I think your shoulder pain is likely tendonitis. We’re going to send you for an MRI to confirm, and I’ll prescribe an anti-inflammatory to help in the meantime. We’ll follow up in 6 weeks.” This not only reassures the patient by summarizing the visit, it also means the AI has a nicely structured plan to write up. I don’t worry if I didn’t vocalize “internal rotation 30°” or a detailed review of systems – that stuff, if important, I’ll handle in a moment. The patient leaves with a clear understanding of the plan (bonus: better patient satisfaction, which some studies have noted when AI scribes let doctors make more eye contact[5]).
After the encounter, add details and corrections via dictation: Once the patient leaves and I’m in a quiet space, I resume talking to the scribe to fill any gaps. This is where I’ll plug in all those specifics I didn’t say aloud. I might mutter, “Physical exam, addendum: The left hip had 120° flexion, internal rotation 30° with mild pain, no instability. Neurologic exam: strength 5/5 throughout, sensation intact.” I can also coach the AI to adjust the note. For example, I might say, “Emphasize that the patient’s neurological exam was completely normal.” Or, “Add a statement that we provided a work excuse note for 2 days.” Essentially, I’m treating the AI like a live scribe whom I can give instructions: “Make sure to include this, make that more clear.” Modern ambient AI systems are surprisingly adept at incorporating these kinds of commands or additional inputs. They won’t always be perfect – sometimes the AI might not 100% obey complex requests – but in many cases I’ll see the final note reflect exactly what I asked for.
By following this before-during-after voice narration approach, I end up with a comprehensive note that required very little typing. The ambient scribe has captured the conversation and my later addenda, and it typically produces a coherent draft that just needs a quick review. Importantly, this method keeps the patient encounter itself patient-centered. I’m looking at them, not a screen or a notepad, aside from brief asides to mention key findings. Patients often comment how much eye contact and listening I’m doing – little do they know, an AI assistant is diligently taking notes in the background the whole time.
To use a financial analogy, leveraging your voice this way is like compounding interest on your time – you invest a bit of extra narration and get a huge return in saved typing and clarification later. And it takes advantage of the fundamental speed difference between speaking and typing. Why slog through typing or clicking checkboxes for 10 minutes after the visit if you can speak the same content in 2 minutes? When you iterate on what you’ve spoken (with the AI refining each version), your documentation process accelerates dramatically. I like to say expressive voice is a clinician’s superpower in the age of AI.
Limitations: What Ambient Scribes Won’t Do (Yet)
Before we look to the future, it’s worth noting a few things ambient scribes don’t do well at present. Understanding these limitations helps you know where you still need to pay attention or supplement the AI.
They only document what’s said (obvious but important): If something is left unspoken, the AI won’t miraculously include it. This sounds trivial, but consider the many implicit or non-verbal cues in a visit. An ambient scribe can’t note that the patient looked anxious when discussing their diagnosis, or that they grimaced when you pressed on their abdomen, unless you explicitly speak it. More concretely, there are billing and compliance phrases that we clinicians have learned to include for reimbursement or medicolegal reasons – e.g. “total time spent face-to-face counseling the patient ___ minutes” or specific MDM (medical decision making) verbiage. The AI won’t know to add those magic words unless you prompt it. Many of the current systems were not trained on the nuances of billing documentation, so you must ensure those elements make it into the note yourself. Similarly, prior authorization landmines – certain keywords that head off insurance denials – aren’t reliably recognized by AI scribes yet. It’s wise to double-check that any phrasing needed for coverage or justification is present before you sign the note.
They can miss or omit details from the conversation: AI transcription isn’t perfect. While ambient AI models have impressively low error rates for medical speech overall (~1–3% error, better than older voice dictation)[15], they do make mistakes. Apart from mis-hearing words, a bigger issue can be omissions – the AI might simply skip over a detail that was said if it deems it unimportant or if the audio was unclear. A recent commentary noted that even with AI scribes, critical information discussed can fail to appear in the note[16]. For example, if the patient mentions a symptom in passing and you acknowledge it verbally but move on, the AI might leave it out of the summary. Always give your AI-generated note a brief review to catch any such omissions or inaccuracies (ultimately, you are responsible for the record’s accuracy). And remember that non-verbal info is entirely lost – if something visual or tactile was clinically significant, you need to say it out loud or add it later. The AI also can’t infer context that wasn’t discussed; it only knows what’s in the conversation.
They may introduce errors (“hallucinations”) or mix up who said what: Although rare, AI scribes have been known to occasionally fabricate plausible-sounding sentences that no one actually said – a phenomenon called hallucination[17][16]. This might be something benign like stating a test was ordered when it wasn’t, but it could also be more serious (documenting a diagnosis that was never discussed, for instance). These systems can also confuse speaker attribution, especially if multiple people are talking (e.g., a patient, a physician, and a nurse practitioner chiming in)[18]. The note could accidentally attribute a patient’s comment to the clinician or vice versa. Again, vigilance during your review is necessary. The good news is that when physicians do review AI notes, studies have found the final documentation ends up higher quality than physician-generated notes alone[19]. The AI handles the first draft, but our human oversight corrects the occasional errors. It’s a partnership – just one where the human must do the final sign-off.
They are not a replacement for clinical judgment or completeness: An ambient scribe won’t decide for you what needs to be documented. It will draft what it hears, but you set the agenda. If you forget to address something in the visit, the AI won’t magically fill it in. It’s still up to us as clinicians to ensure the note reflects the clinically relevant points, the rationale for decisions, and any required counseling or follow-up instructions. Think of the AI as an efficient clerk, not a practicing physician. It can help record your decisions, but it can’t make them. And if there are specific phrases your note needs (for legal or billing reasons), you might still need to insert those manually as mentioned. In short, ambient scribes greatly reduce the clerical burden, but they don’t relieve us of our role as the final editor and decision-maker for the content.
Finally, a brief word on patient privacy and comfort. While most patients adapt well to the idea of an AI scribe (especially when it means their doctor is more attentive), always be prepared to turn it off if a patient is uncomfortable. Sensitive topics like mental health, domestic violence, or sexual history might warrant pausing the recording – use your judgment[20][21]. From a legal perspective, as noted earlier, ensure you comply with recording consent laws in your jurisdiction and your health system’s policies. The last thing you want is a privacy complaint. These tools are designed to be HIPAA-compliant (many don’t store raw audio or they encrypt it such that only the transcript is saved), but transparency with patients is key to maintaining trust.
The Next Frontier: From Documentation to Conversation-Driven Care
Ambient AI scribes today are primarily a documentation aid – a “wedge” into the clinical workflow that starts by solving the note-taking problem[22]. But their implications extend much further. By capturing the rich data in conversations, we have an opportunity to fundamentally improve care delivery. After all, communication is the bedrock of medicine: the history we take, the explanations we give, the rapport we build – these are all conveyed in conversation. For the first time, technology allows us to record and analyze that layer of healthcare at scale.
What might this enable? One exciting area is clinical outcomes and quality improvement. Imagine analyzing thousands of doctor-patient dialogues to see what patterns lead to better outcomes. Are there phrases or counseling approaches that result in higher patient adherence? Could we identify when a crucial symptom was mentioned but not acted upon? In fact, research has already shown huge gaps between what is verbally discussed and what ends up in the chart – one study found ~50% of patient problems brought up in home health visits never got documented in the official record[23]. Capturing conversations could help close that documentation gap, ensuring important issues aren’t lost to memory. Over time, linking conversation content to outcomes (like controlling chronic disease, avoiding readmissions, patient satisfaction scores, etc.) could teach us which communication strategies truly make a difference.
We’re already seeing ambient scribe companies move in this direction. Some platforms are augmenting their note-taking with features for clinical coding and billing – essentially translating conversation directly into proper ICD-10 codes and billing-ready documentation. For example, Ambience Healthcare’s ambient AI not only writes the note but also auto-generates content for clinical documentation integrity (CDI), ICD-10 coding, and even prior authorization forms as part of its platform[24]. This hints at a future where the AI doesn’t just help produce a narrative, but actually handles the bureaucratic follow-ups (like justifying a CT scan to an insurance company) based on the conversation. Abridge, the company I mentioned earlier, explicitly talks about embedding “revenue cycle intelligence” into the point of care – recognizing that the note it generates is essentially the bill, and optimizing it accordingly[25]. When Shiv Rao MD, Abridge’s CEO, says “we are, in essence, a mid-revenue cycle company”[25], it underscores that ambient AI is expanding from note-taking into the financial and operational side of care.
Beyond billing, consider care coordination and gap closure. An ambient scribe could alert a care navigator if, say, a cancer screening wasn’t discussed during a visit where it should have been, or automatically generate a follow-up task if a patient mentioned an unresolved issue (“I’ve been feeling more short of breath lately…”) that didn’t get fully addressed. Some forward-thinking teams (including ours at my institution) are already experimenting with linking ambient scribe data to patient outreach. We have begun pairing patient-facing AI agents (for example, a chatbot that checks in on patients between visits or collects pre-visit information) with the clinician-facing ambient scribe. The result is a more continuous loop of communication. The patient tells the chatbot something which informs the visit; the ambient scribe records the visit and flags something for the care team to follow up on later. It’s not hard to imagine this ecosystem improving chronic disease management or post-surgery recovery by making sure nothing falls through the cracks. The ambient scribe becomes not just a documentation tool, but a context engine that ties together all the conversations happening in a patient’s journey.
And what about surgery, or other areas currently untouched by ambient tech? I’m a surgeon myself, and I suspect the next big push may be into operative notes. Today, most surgeons dictate their op notes in a fairly rote manner to satisfy billing (certain keywords can make the difference in coding a complex procedure). An AI that could learn each surgeon’s style and generate a compliant op note could be a game-changer for hospital efficiency. The challenge is that ORs have their own workflow, and surgeons can be a traditional bunch – I’ve seen some bristle at the idea of deviating from their trusted dictation routine. However, as the technology improves and perhaps offers verbatim modes or highly customizable outputs, we may see ambient scribes scrubbing into the OR too. It’s an area ripe for innovation, given how formulaic yet critical operative reports are. The first companies to crack the “AI surgical scribe” in a way that truly understands procedural nuances (and doesn’t miss those all-important billing phrases) will have a compelling product.
In closing, it’s worth reflecting on how quickly ambient AI scribing went from novelty to near-commodity. There are many players with seemingly similar offerings, and as one health tech author quipped, the core transcription capability is becoming commoditized. But what’s not a commodity is the value of the data and insights that lie in our clinical conversations. In my view, the real winners in this space will be those who leverage ambient scribing as the foundation for something bigger: improving clinical workflows and outcomes. We started with solving physician burnout (a worthy goal on its own – and largely being achieved, as burnout rates are dropping where these tools are used[26][27]). The next step is to translate the countless hours of conversation now being captured into actionable knowledge. This could mean identifying unmet needs, automating routine tasks (like drafting patient instructions or referral letters), or even surfacing behavioral cues that predict which patients might struggle with their treatment plans.
Healthcare, at its heart, is still about people talking to people – the doctor-patient relationship, the care team communication. Ambient AI is giving us a new lens on those interactions and, arguably, a way to enhance them by removing distractions. The clinic of the future might have AI “colleagues” quietly listening in on every consult, not only writing notes but coordinating care and learning what works best. It’s a future where technology truly fades into the background, as one CMIO described it, “allowing care to come to the foreground”[28]. We’re not quite there yet, but if you use your clinic’s ambient scribe to its fullest potential today – freeing up your time and mental bandwidth – you’re already laying the groundwork for that transformation.
For Paid subscribers, I have an interactive landing page of this website, as well as the prompt I used in GPT to create the landing page in Gemini. Vibe coding has serious limitations, and we’re seeing a major slowdown in the growth of these hyped up tools, but I think interactive content and prototypes are still incredibly useful. I just used google’ gemini tools to create these. See below!
Techy Surgeon Vibe Coded Interactive Landing Page on Ambient Scribes
Keep reading with a 7-day free trial
Subscribe to Techy Surgeon to keep reading this post and get 7 days of free access to the full post archives.