The ACCESS Model, Explained
Part 1 of a 12-part operator series on the CMS ACCESS Model
There has been no shortage of commentary since CMS released the 61-page Request for Applications for the ACCESS Model.
The early reactions were predictable. Medicare finally opens to digital health. A direct threat to fee-for-service. A gold rush for chronic disease management.
I shared my initial impressions shortly after the RFA dropped and created a landing page at TechyPolicy.com for readers who wanted to track the model more closely as details emerged.
Those headlines are not wrong. But they are incomplete.
What CMS has not yet released are the numbers that usually dominate these conversations. We still do not know the per-beneficiary outcome-aligned payment amounts. CMS has said those figures will come in 2026. What the agency has provided instead is something more revealing: a detailed architecture of participation that shows who can realistically enter the model, what participation requires, and where the economic tensions sit.
That architecture will matter as much as the payment itself.
The short video above walks through how I am thinking about ACCESS at a structural level. Not whether the model is ambitious or disruptive, but whether it can function as designed once real organizations with real incentives attempt to operate inside it.
What the explainer covers
Why ACCESS is being interpreted as a direct Medicare entry point for digital health companies
The Part B enrollment requirement that separates interest from eligibility
The fee-for-service exclusion rule and why it reshapes health system participation
The coordination problem created when patients receive care across overlapping payment models
The central tension
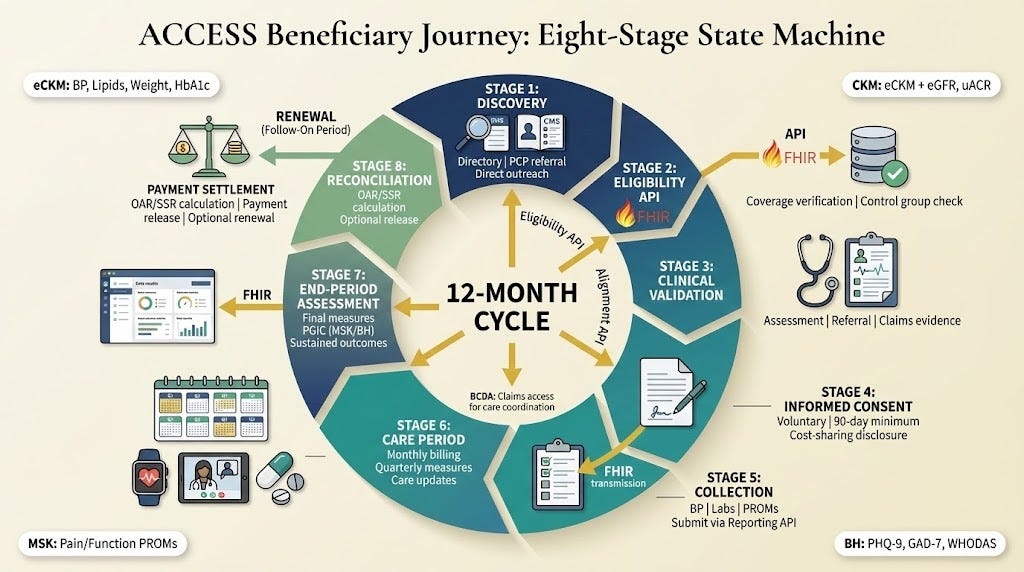
ACCESS introduces something genuinely new for Medicare. Chronic care delivered through technology-enabled models, paid on outcomes rather than visits.
But the constraint that defines the model is easy to miss.
Buried in the RFA is a clear rule: ACCESS participants and their affiliates cannot bill Medicare fee-for-service for aligned beneficiaries during active care periods.
For organizations without existing fee-for-service revenue, this is not an obstacle. It is the design feature that makes the model viable. Outcome-aligned payment replaces visit-based billing rather than competing with it.
For health systems whose economics still depend heavily on fee-for-service billing, the math looks very different. Participation does not require regulatory exclusion. It creates financial exclusion on its own.
The likely result is selective participation rather than universal adoption. Patients may be enrolled with one organization for ACCESS conditions while continuing to receive primary care or specialty services from others operating under entirely different incentives.
In that environment, coordination is not a secondary consideration. It is the model.
What we still do not know
Several core elements of ACCESS remain unresolved.
CMS has not yet published per-beneficiary payment amounts by clinical track. The details of the risk adjustment methodology remain unclear. It is also not yet known how outcome attainment thresholds will evolve beyond the first performance year.
What we do know are the timelines.
Applications open in January 2026. The initial deadline is April 1. The first cohort launches July 5, 2026.
That leaves organizations roughly a year to decide whether ACCESS fits their strategy, and if so, how to structure participation without creating unintended exposure.
About this series
This post is the first in a 12-part series examining the ACCESS Model from an operator’s perspective.
Each installment focuses on one specific mechanic in the RFA and the practical implications CMS does not always state explicitly. The goal is not advocacy for or against the model, but clarity around how it functions once contracts are signed and patients are enrolled.
New posts will publish on TechyPolicy.com throughout the series.
If you want a brief downloadable overview of the model, download the PDF here. I’ll have more operator-specific and mechanics-specific resources and assets throughout the course.
Follow the 12-part ACCESS series
I’ll be releasing an article a day and explaining topics. Paid subscribers receive all posts, diagrams, and decision frameworks.
A note on coordination infrastructure
For transparency, I am co-founder and CEO of RevelAi Health. We build care coordination and patient engagement infrastructure designed for value-based and outcome-aligned models.
ACCESS will require reliable outcome measurement, sustained patient engagement, and real communication across organizational boundaries. Those capabilities will determine whether coordination succeeds or breaks down.
If you are evaluating ACCESS and want to talk through the operational requirements, I am open to those conversations.
📧 hello@revelaihealth.com
🌐 www.revelaihealth.com